How Nutrition Can Support Clients Using GLP-1 Medications
GLP-1 medications such as Mounjaro, Wegovy and Ozempic are increasingly being used to support weight loss and blood sugar regulation. While these medications can be powerful tools, they are not a standalone solution. Nutrition plays a critical role in improving results, minimising side effects, and supporting long-term health and weight maintenance.
As a nutritional therapist, I often see that the clients who feel best and achieve the most sustainable outcomes are those who combine GLP-1 therapy with targeted nutritional support.
Understanding What GLP-1 Medications Do
GLP-1 medications work by mimicking the action of the naturally occurring hormone glucagon-like peptide-1. This hormone plays a key role in appetite regulation, digestion and blood sugar control.
One of the primary effects of GLP-1 medications is slowing gastric emptying, meaning food stays in the stomach for longer. This enhances feelings of fullness and satiety after meals, often leading to smaller portion sizes and reduced snacking. While this can support calorie control and weight loss, it may also increase the likelihood of nausea, bloating, reflux or a heavy feeling after eating, particularly if meals are large or poorly balanced.
GLP-1 medications also act on appetite centres in the brain, helping to reduce hunger signals and food cravings, especially for highly palatable, ultra-processed foods. For many people this can feel like a welcome relief from constant thoughts about food. However, a significantly reduced appetite can make it more challenging to consume adequate protein, fibre and essential micronutrients, increasing the risk of fatigue, muscle loss and nutrient deficiencies over time.
In addition, GLP-1 medications help to improve insulin sensitivity and blood sugar regulation. They enhance insulin secretion in response to meals and reduce inappropriate glucose release from the liver, supporting more stable blood sugar levels. While this is beneficial for metabolic health, blood sugar balance still relies heavily on food quality, meal composition and timing. Poorly structured meals or prolonged periods of undereating can still lead to energy dips, dizziness and cravings.
Although these combined effects can be highly effective for weight loss and metabolic improvement, they also increase the likelihood of unintended consequences such as reduced overall food intake, digestive discomfort, constipation, low energy and nutrient shortfalls—particularly if nutrition is not proactively addressed.
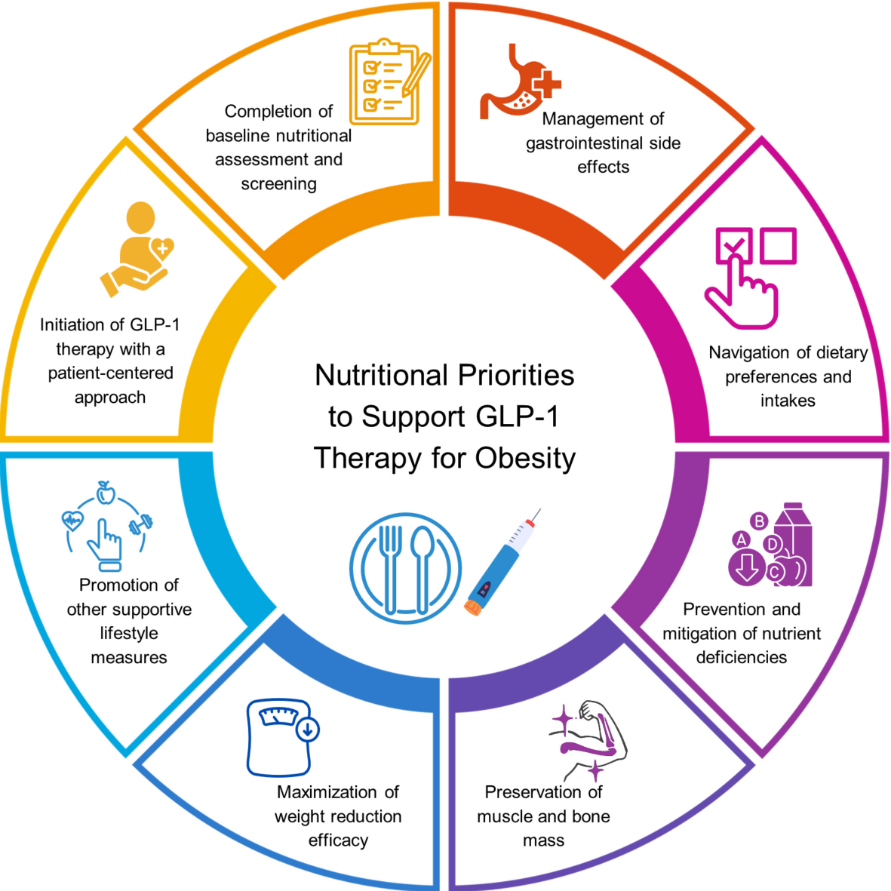
This is where personalised nutrition becomes essential. Tailored nutritional support helps ensure that even with a reduced appetite, the body receives adequate protein, key micronutrients and digestive support. It also helps minimise side effects, protect muscle mass, stabilise energy levels and support long-term metabolic health, creating a safer and more sustainable approach alongside GLP-1 therapy.
Why Nutrition Matters Alongside GLP-1 Therapy
Prevents Muscle Loss and Metabolic Slowdown
Rapid weight loss without adequate protein intake significantly increases the risk of lean muscle loss, not just fat loss. Loss of muscle tissue is particularly important to avoid, as muscle plays a key role in metabolic health, strength and long-term weight regulation. When muscle mass is reduced, it can:
Slow resting metabolic rate, meaning the body burns fewer calories at rest
Reduce physical strength, stamina and overall energy levels
Increase the likelihood of weight regain once medication is reduced or stopped, as the body becomes more metabolically efficient at storing energy
A nutrition plan that prioritises sufficient, high-quality protein, evenly distributed across meals and snacks, helps preserve lean muscle mass during weight loss. This approach also supports satiety, blood sugar stability and metabolic health, making weight loss safer, more sustainable and easier to maintain long term.
Supports Digestive Comfort and Gut Health
GLP-1 medications can commonly affect digestive function due to their impact on gastric emptying and appetite regulation. As a result, some clients experience symptoms such as:
Nausea, particularly if meals are too large or eaten too quickly
Bloating or abdominal discomfort
Constipation or sluggish digestion due to reduced food volume and slower gut motility
Acid reflux or a feeling of food sitting heavily in the stomach
Targeted nutritional support can significantly reduce these symptoms and improve day-to-day comfort. This may include:
Choosing easily digestible, nutrient-dense foods that are gentler on the digestive system
Adjusting meal size, texture and timing to suit slower digestion and reduced appetite
Supporting gut motility with appropriate fibre intake, adequate hydration and key micronutrients such as magnesium
Identifying and temporarily limiting foods that may worsen symptoms, such as high-fat, very fibrous or highly processed foods
Maintaining a healthy gut is not only important for digestive comfort but also plays a key role in appetite regulation, inflammation control and mental wellbeing, all of which support more sustainable outcomes while using GLP-1 therapy.
Avoids Nutrient Deficiencies
Because appetite is significantly reduced on GLP-1 medications, many clients unintentionally under-consume essential nutrients, even when food choices appear healthy. Commonly affected nutrients include:
Protein, which is critical for muscle preservation, metabolic health and satiety
Iron, needed for oxygen transport, energy levels and cognitive function
B vitamins, which support energy production, nervous system health and hormone balance
Magnesium, important for muscle function, stress regulation and digestion
Zinc, essential for immune function, wound healing and appetite regulation
Omega-3 fats, which support inflammation control, cardiovascular health and brain function
Over time, these nutrient shortfalls can contribute to a range of symptoms, including:
Persistent fatigue or low energy
Hair thinning or poor hair quality
Low mood, brain fog or reduced stress resilience
Poor recovery from exercise or daily activity
Hormonal disruption, including changes to menstrual health
Personalised nutrition ensures that every bite counts, focusing on nutrient-dense food choices and appropriate supplementation where needed. This approach helps deliver maximum nourishment, even with smaller portions, supporting overall health, energy and long-term success alongside GLP-1 therapy.
Improves Blood Sugar Stability and Energy Levels
Although GLP-1 medications help improve insulin sensitivity and support blood sugar regulation, food choices still play a crucial role. Meals that are low in protein or fibre, or overly reliant on refined carbohydrates, can still lead to fluctuations in blood glucose levels. This may result in:
Blood sugar dips between meals
Dizziness or light-headedness
Increased cravings, particularly for quick sources of energy
Low or unstable energy levels throughout the day
A nutrition plan focused on adequate protein, fibre-rich carbohydrates, healthy fats and overall micronutrient density helps promote steadier blood sugar responses. This approach supports sustained energy, improved satiety and reduced reliance on ultra-processed foods, allowing GLP-1 medications to work more effectively alongside long-term metabolic health.
Supports Long-Term Weight Maintenance
One of the biggest concerns with GLP-1 medications is weight regain after stopping treatment, particularly if rapid weight loss has occurred without addressing underlying habits, metabolic health and the relationship with food.
Ongoing nutrition support helps clients to:
Build sustainable eating habits that can be maintained beyond medication use
Improve metabolic flexibility, supporting the body’s ability to efficiently use both carbohydrates and fats for fuel
Address emotional and stress-related eating, which is often unchanged by medication alone
Reconnect with natural hunger and fullness cues, rather than relying solely on appetite suppression
Develop renewed confidence around food choices, portion sizes and meal timing
Together, these factors create a strong, supportive foundation for maintaining results long after medication is reduced or discontinued, helping weight loss feel more sustainable, empowering and health-focused rather than temporary.
Nutrition Is Not About Eating Less, it’s About Eating Smarter
GLP-1 medications can significantly change appetite and eating patterns, but they do not teach the body how to nourish itself optimally. Appetite suppression alone does not guarantee nutritional adequacy, metabolic resilience or long-term health. Nutrition bridges this gap by providing the body with the tools it needs to adapt and thrive during weight loss.
Targeted nutritional support helps to maintain:
Physical health, by preserving muscle mass and preventing nutrient deficiencies
Digestive comfort, by reducing common side effects and supporting gut function
Hormonal balance, which is closely linked to energy levels, mood and metabolic health
Mental wellbeing, by supporting brain chemistry, stress resilience and a healthier relationship with food
Long-term success, by building habits that support weight maintenance beyond medication use
When medication and nutrition work together, outcomes are not only more effective, but also safer, more comfortable and far more sustainable, supporting both short-term results and long-term wellbeing.
If you’re using a GLP-1 medication and want to feel your best while achieving lasting results, working with a nutritional therapist can make all the difference.
Book your free clarity call if you’d like more information on how a nutritionist could help you on your GLP-1 medication journey.